From Primary Lateral Sclerosis (PLS), and Signs of Illness
This page explains the technical reason that after twelve years of a disease extremely close to ALS I still am blessed to have very strong muscles. It’s all in the distinction between Upper and Lower Motor Neurons. My condition involves almost exclusively the Upper Motor Neurons with almost no involvement of Lower Motor Neurons. This distinction is explained more fully below in an article from the ALS Association web site.
Ask the Doc: Q & A with Edward Kasarskis, MD, PhD
Edward Kasarskis, MD, PhD is Director of the University of Kentucky ALS Multidisciplinary Clinic at Cardinal Hill Rehabilitation Hospital in Lexington, Kentucky, professor in the Department of Neurology at the University of Kentucky, and Chief of Neurology at the VA Medical Center in Lexington KY.
From the ALS Association website October 2010
Q: My 38-year old brother was diagnosed one year ago. On his only visit to the ALS clinic so far his doctor told him that his situation was mostly “upper neuron.” What does this mean? He barely walks and has no use of his hands (where the symptoms started). His speech has all but disappeared. What is the difference between upper motor neuron disease and lower motor neuron disease? What gets affected the most, and when?
A: This is a very good question and is basically about classifying your brother’s disease. To understand what his doctor was trying to convey, we first need an understanding of some terminology and concepts as they apply to the organization of the brain, spinal cord, and voluntary muscle. This is about to become a bit complicated, so hang in there with me.
You probably already know this, but . . . muscle weakness in ALS is caused by the degeneration, dysfunction, and death of motor neurons — not because of a defect in the muscle itself. Neurons are nerve cells; motor neurons are nerve cells involved in producing movement. For this reason, ALS is frequently referred to as a “Motor Neuron Disease” (MND). So, how do motor neurons produce movement?
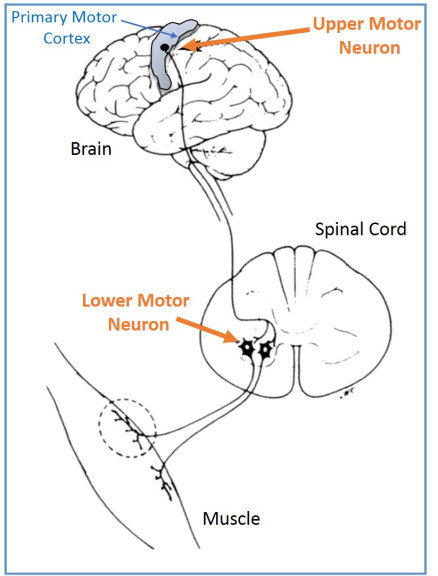
Any movement begins with an idea and plan formulated in the brain—walk to the bookstore, play with the cat, get a beer, etc. The motor plan eventually converges on the motor neurons in the motor cortex of the brain. These are the so-called, “upper motor neurons” (UMN) or “Cortical Motor Neurons.” Let’s say you are going to move your right hand. The UMNs residing in the “hand region” of the motor cortex on the left side of your brain control movement of the right hand.
But that is only the beginning of the story. These are huge nerve cells whose body is in the motor cortex but part of the neuron known as its “axon” physically extends downward from the top of the brain, passing through the brain, crossing over to the right side, and contacting a second set of motor neurons in the cervical spinal cord in the neck area. So this single UMN is, in reality, probably 1-2 feet in length.
As you probably have guessed, the spinal motor neurons are the “lower motor neurons” (LMN). The LMN is similarly huge. The cell body of the LMN resides in the spinal cord but its axon leaves the spinal cord and goes out to the arm in this example and contacts the muscles in the arm that move the right hand. There are many other neurons involved in creating and smoothing movement, but the basic set up of UMN to LMN to muscle is all we need to consider in ALS. So to move the hand, the UMN electrically fires off a signal to the LMN, which fires of a second electrical signal to the muscles, which are stimulated to contract causing movement.
How do we neurologists know that we have a problem involving the UMN or LMN? A physical exam typically finds different signs and symptoms depending on whether you have upper or/and lower motor neuron degeneration. Signs of UMN disease usually include spasticity of the muscles (a stiffness and resistance to movement), brisk reflexes and a Babinski sign, (a reflex that is a sign of damage to the nerve paths connecting the brain to the spinal cord). Signs of LMN damage include weakness, muscle atrophy (wasting), and fasciculations (muscle twitching). These signs can occur in any muscle group, including the arms, legs, torso, and bulbar region.
In classical ALS, a person experiences both UMN and LMN signs in the same region, for example in an arm. However, there is a spectrum of involvement within a region. Sometimes people who have symptoms predominantly associated with UMN disease, so the picture is one of tremendous spasticity and slow movement. However an EMG test will give evidence of the LMN component of ALS. This is probably the situation in the case of your brother, the so-called upper motor neuron predominant ALS. A rare person may only have UMN involvement without any LMN dysfunction. In the US, we would label this condition as “Primary Lateral Sclerosis” (PLS). On the other side of the MND spectrum, another person may only have LMN signs with minimal UMN findings.
Whichever type of MND a person has, the anticipation is that the condition will progress. As such, all will face problems with mobility, speech and communication, swallowing dysfunction, and ventilatory insufficiency. Careful follow up is needed to manage these problems as we have discussed previously in this column.
From the ALS Association website October 2010